| Type of paper: | Essay |
| Categories: | Health and Social Care Food Society |
| Pages: | 6 |
| Wordcount: | 1426 words |
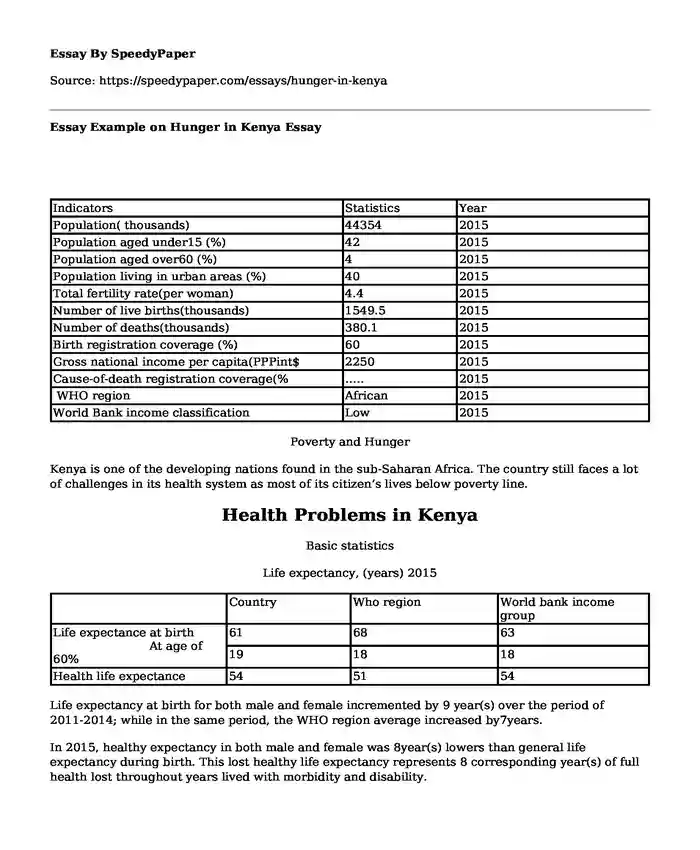
| Indicators | Statistics | Year |
| Population( thousands) | 44354 | 2015 |
| Population aged under15 (%) | 42 | 2015 |
| Population aged over60 (%) | 4 | 2015 |
| Population living in urban areas (%) | 40 | 2015 |
| Total fertility rate(per woman) | 4.4 | 2015 |
| Number of live births(thousands) | 1549.5 | 2015 |
| Number of deaths(thousands) | 380.1 | 2015 |
| Birth registration coverage (%) | 60 | 2015 |
| Gross national income per capita(PPPint$ | 2250 | 2015 |
| Cause-of-death registration coverage(% | ….. | 2015 |
| WHO region | African | 2015 |
| World Bank income classification | Low | 2015 |
Poverty and Hunger
Kenya is one of the developing nations found in the sub-Saharan Africa. The country still faces a lot of challenges in its health system as most of its citizen’s lives below poverty line.
Health Problems in Kenya
Basic statistics
Life expectancy, (years) 2015
| Country | Who region | World bank income group | |
| Life expectance at birth At age of 60% | 61 | 68 | 63 |
| 19 | 18 | 18 | |
| Health life expectance | 54 | 51 | 54 |
Life expectancy at birth for both male and female incremented by 9 year(s) over the period of 2011-2014; while in the same period, the WHO region average increased by7years.
In 2015, healthy expectancy in both male and female was 8year(s) lowers than general life expectancy during birth. This lost healthy life expectancy represents 8 corresponding year(s) of full health lost throughout years lived with morbidity and disability.
Source: Country statistics and global health estimates by WHO and UN partners
Global Health Issues and Indicators Observed
Health indicators have been inextricably linked to poverty and hunger which are some of the global health issues that continue to be experienced. The causes of poor health for millions of people worldwide are rooted in social, political and economic injustices especially in third world countries. Poverty is both a consequence and a cause of poor health in most developing countries. The community is then trapped into poverty as a result of poor health as most people are not able to work when they are feeling unwell. Every year, infectious and tropical disease that has been ignored weaken majority of individuals in marginalized and poor communities (Study.com ,2013-2016).
Furthermore, poverty has led to poor overcrowded and poor living conditions which have drastically contributed to the spread of airborne disease such as tuberculosis and pneumonia which are respiratory infections. Notably, most communities living in poverty rely on traditional stoves and open fire as sources of energy which have proved to be indoor air pollution. Studies have shown that most of the poverty stricken communities still believe in social and cultural norms which sometimes act as barriers while accessing medical services. As such, very few individual ends up using health centres as another relay on traditional medicines which does not cure various deadly diseases World Health (Organization, 2016).
Marginalized societies are made up of individuals who are most affected, vulnerable and have no money to access health services. Global health issues have been experienced more in African countries; studies indicate that 300 mothers in Africa loose a small every hour. In 2014, more than 3.5 million African children lost their life. The increased number of deaths are directly associated with poverty and hunger. Furthermore, lack of medical services in the grass root level has been a key contributor to some of these deaths as some of them could have been prevented. Women are forced to stay at home with these children as they lack money to travel for long distances to seek medical services (Jamison,2015).
Structure of Health System in Kenya
Considering the hierarchical structure of Kenyan health system, basically, the health system of Kenya is governed from the top level down to the bottom level by the ministry of health. The system is composed of various institutions like Kenya’s health system is composed of health centers, dispensaries, nursing homes and sub-district hospital, private and district hospital, provincial and national level hospitals. Critically, talking about the Kenyan experience, splitting of health sector into various sections has at one point caused inefficiency and overlapping in both the implementation process and the planning process. The availability of the best and the most sophisticated health services are present in the national level hospital, with the next best level of health care experienced at the provincial level and then the sub-district hospitals. Due to a little contribution of government funding and support o the lower level which is the dispensaries and health sectors, the community organizations and dispensaries recorded the least care of attention (Mohajan, 2014).
Notably, the government of Kenya has incorporated and allowed support from the NGO into their health system. The overall national health system is controlled by the National Health Sector Strategic Plan II(NHSSP II) ,and its depending on the Sector Wide Approach(SWAp) that has the purpose of integrating the public health care and the private health care to work in a unifying manner.
Basically, in reference to the world health organization, one of their popular report revealed that Kenya, a country with more than thirty million individuals is seriously struggling to develop a health system that can efficiently and effectively provide quality health services to the individuals. In some cases, some individuals have no access to health care and they only know about the traditional methods of treatment. Due to an increasing level of poverty in Kenya, some parts of the country have no access to proper accessibility hence it’s difficult to supply medicine and health staffs. Basically, the average life expectancy in Kenya, fall between fifty-four to fifty-six percent which is totally different from the global average life expectancy rate which is sixty-eight. Technically, the less than four years mortality rate falls between the populations of one hundred and twenty-one per every one thousand live births even drop to one hundred and fifty for the poorest twenty percent. This is generally contributed by hunger and poverty which is experienced in the country hence the poor suffer most (Mohajan, 2014).
Health Care System of Kenya
Generally, in Kenya, better healthcare, and technical medical instruments are only available in the national health care institutions and some of the private medical sectors. This basically makes the limit most population of Kenyan individuals at the grassroots level to be able to seek medical attention. Actually, the national level is situated in most big cities which can only be accessed by a small population who can be able to afford the healthcare. Since most of the Kenyan population is poor, the cannot afford the expensive and better medical care being offered in most cities hence technically, the high death rate is being experienced in this country (Nonvignon et al.2016)
In some of the provinces like northeastern, the government has not even made serious efforts to manage their major problems like lack of water supply and frequent food supplies. Technically, they are not able to send technical health staffs and medical care services to take care of their individuals in marginalized areas. The life expectancy rate is very low with frequent high mortality rate. Some of these areas cannot be supplied by proper medicine and health care since they are not accessible enough to be penetrated; there exist a lot of poor roads and the higher level of insecurity issues. Most children in the North Eastern die at a younger age as a result of high level of poverty and hunger, the area is a semi-desert with little food and water, hence most of the children are generally dying because of poor medication and hunger. Though most NGOs have tried their best to penetrate these areas, poverty and hunger are still dominating and a challenge (Aidam at el,2016)
References
Aidam, B. A., Edward, A., Paden, A. C., Wong, R. Y., & Chege, J. (2016). Addressing Anemia in Women and Children in Rural Communities of Cambodia and Kenya: Experiences from an Integrated Program. The FASEB Journal, 30(1 Supplement), 892-12
Jamison, D. T. (2015). Disease Control Priorities: improving health and reducing poverty. The Lancet.
Mohajan, H. K. (2014). Improvement of Health Sector in Kenya. American Journal of Public Health Research, 2(4), 159-169
Nonvignon, J., Mensah, E., Vroom, F. B. D. C., Adjei, S., & Gyapong, J. O. (2016). The Role of Health Systems in the Control of Neglected Tropical Diseases in Sub-Saharan Africa.
In Neglected Tropical Diseases-Sub-Saharan Africa (pp. 385-405). Springer International Publishing
Study.com (2013-2016). Risk Factors for Contracting Communicable Diseases. Retrieved from: http://study.com/academy/lesson/risk-factors-for-contracting-communicable-diseases.htm
World Health Organization (2016). Global infectious disease surveillance Retrieved from: http://www.who.int/mediacentre/factsheets/fs200/en
World Health Organization (2016). Communicable diseases in the South-East Asia Region of the World Health Organization: towards a more effective response.
Cite this page
Essay Example on Hunger in Kenya. (2017, Oct 18). Retrieved from https://speedypaper.net/essays/hunger-in-kenya
Request Removal
If you are the original author of this essay and no longer wish to have it published on the SpeedyPaper website, please click below to request its removal:
- Movie Review in a Free Essay: Skiptrace by Jackie Chan
- Arguments against the Death Penalty - Essay Example
- Essay Example: Incorporating Patients in Decision-Making Process
- Paper Example on Differences Between Teaching Online and In-Person
- Free Essay Example: Creating a Strategic Plan
- Free Essay. "Yesterday's Whales"
- Essay Example: The Importance of Predator-prey Relationships for a Healthy Ecosystem
Popular categories




